Link a member or dependent to PPO
If a plan has multiple PPO![]() A group of providers who contract with employers, insurers or administrators to provide services to individuals for a negotiated amount. options and requires a member to select a PPO, use this option to enter that information.
A group of providers who contract with employers, insurers or administrators to provide services to individuals for a negotiated amount. options and requires a member to select a PPO, use this option to enter that information.
The PPO selection can also be stored at the dependent level. If the claim is
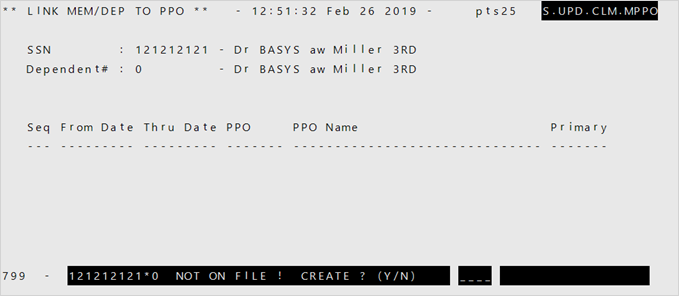
- If the member isn't already associated with a PPO, a message shows at the bottom of the screen asking if you want to create an association. Enter
Y. - Enter the
FromandThru Dates. - Enter the
PPO. Valid values are- UHC—United Health Care
- AL—Alliance PPO
- AETNA—AETNA In-Network
- AETNON—AETNA Out Of Network
- INT—Internal PPO
- If you're entering information on only one PPO for the member, type
1to indicate that this is the member's primary PPO association.- Enter
2or3if this is the member's second or third PPO association.
- Enter
- At the select line, type
F.